EN
2023-11-08
On October 23, in collaboration with Union Laiya and East Hospital, successfully held an academic salon on industry-university-research cooperation for innovative drugs. They had the honor of inviting the original inventor of the BOIN design (the first innovative Phase I clinical study design invented by a Chinese professor and certified by the U.S. FDA)—Professor Ying Yuan, the Bettyann Asche Murray Distinguished Endowed Professor at the MD Anderson Cancer Center, Professor Fangrong Yan, Head of the Department of Biostatistics at China Pharmaceutical University, along with several clinical experts to gather together for exciting interactions with both online and offline audiences.


Dr. Zibao Zhang, General Manager of Union Laiya (Host)
Dr. Zibao Zhang has over 20 years of experience in the biopharmaceutical industry, including technical team management, business development, venture capital investment, and enterprise management. He has been responsible for establishing and managing statistical teams in China for several multinational clinical CRO companies, supporting global clinical study operations; participated in founding a clinical CRO company and helped it develop into a global unicorn enterprise, during which he was mainly responsible for establishing and managing business development teams; he also ventured into the investment field, assisting with resource connections and post-investment management, empowering innovative drug and technical service companies. Currently, his work focuses on comprehensive enterprise management, dedicated to building an international brand and providing high-quality clinical CRO services to clients. Dr. Zibao Zhang holds a Ph.D. in Epidemiology and Biostatistics from Fudan University, an Executive MBA degree from China Europe International Business School, and has studied in the CEIBS Venture Capital Camp program.
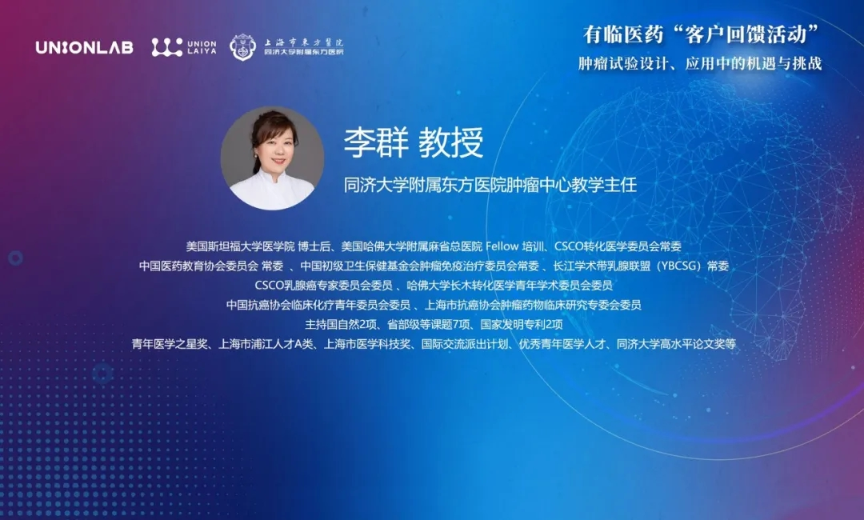
Professor Jin Li, Director of the Department of Oncology, Tongji University East Hospital
President of Shanghai GoBroad Cancer Hospital, Director of the Cancer Research Institute of Tongji University East Hospital, President of the Federation of Asian Clinical Oncology (FACO), Chairman of the CSCO Foundation, Chairman of the Oncology Clinical Research Committee of the China BioMed Innovation and Investment Conference, Vice Chairman of the Oncology Expert Committee for Capacity Building and Continuing Education of the National Health Commission, Former President of the Chinese Society of Clinical Oncology (CSCO), Chairman of the Gastric Cancer Expert Committee of the CSCO, Associate Editor of Cancer Science
Due to being unable to attend in person, Professor Jin Li delivered an inspiring online speech. He stated that Chinese patients urgently need highly effective, low-toxicity, affordable, and convenient drugs that are highly aligned with clinical needs. In addition, to carry out clinical research, scientific prediction and planning are required, with statistics leading the way. He believes that through this event, Professor Ying Yuan, Professor Fangrong Yan, numerous clinical experts, and all participants will certainly spark highly valuable academic insights and solutions to overcome the challenges in the clinical development of anti-tumor drugs. In the future, he hopes that Chinese pharmaceutical companies can go global to allow more patients worldwide to benefit from drugs independently developed by China.

◎ Topic: BOIN Platform to Innovate Early Phase Clinical Studies
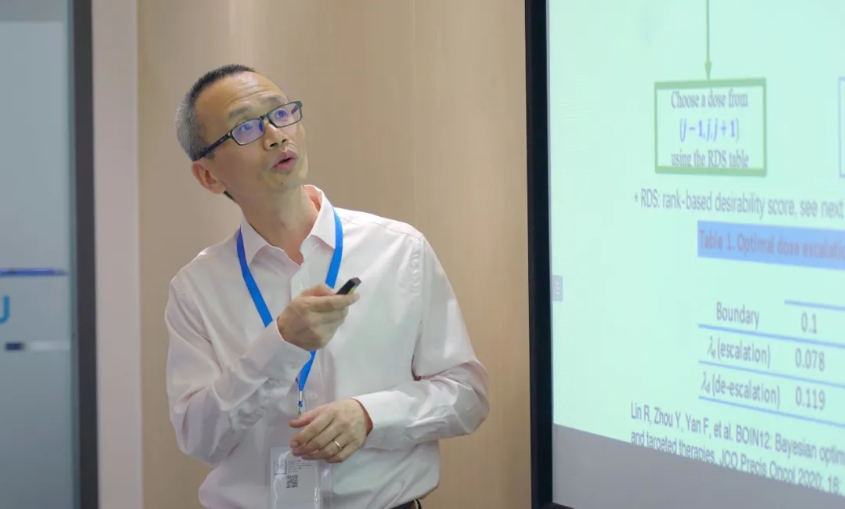
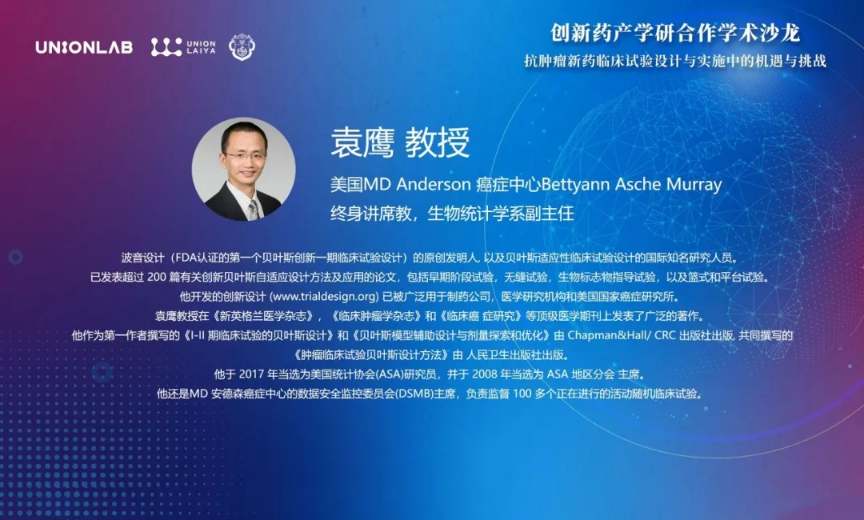
Professor Ying Yuan
MD Anderson Cancer Center, USA
Bettyann Asche Murray Distinguished Endowed Professor
Associate Head of the Department of Biostatistics
Professor Ying Yuan is Bettyann Asche Murray Distinguished Endowed Professor and the Associate Head of the Department of Biostatistics at MD Anderson Cancer Center, USA. He is the original inventor of the BOIN design (the first Bayesian innovative Phase I clinical study design endorsed by the FDA) and an internationally renowned investigator in Bayesian adaptive clinical study designs. He has published over 200 papers on innovative Bayesian adaptive design methods and applications, including early-phase trials, seamless trials, biomarker-guided trials, as well as basket and platform trials. The innovative designs he developed (www.trialdesign.org) have been widely used by pharmaceutical companies, medical research institutions, and the National Cancer Institute. Professor Ying Yuan has published extensively in top medical journals such as The New England Journal of Medicine, Journal of Clinical Oncology, and Clinical Cancer Research. He is the first author of "Bayesian Designs for Phase I-II Clinical Studies" and "Bayesian Model-assisted Designs for Dose Finding and Optimization," both published by Chapman & Hall/CRC, and co-authored "Bayesian Design Methods for Oncology Clinical Studies" published by People's Medical Publishing House. He was elected Fellow of the American Statistical Association (ASA) in 2017 and served as President of the ASA Local Chapter in 2008. He is also the Chairman of the Data Safety Monitoring Board (DSMB) at MD Anderson Cancer Center, responsible for overseeing over 100 ongoing active randomized clinical studies.
Professor Yuan began by introducing the three types of dose escalation: rule-based designs (transparent, easy to implement, but with poor performance. For example: 3+3 design), model-based designs (superior performance, but less transparent and difficult to implement. For example: CRM, EWOC, BLRM), and model-assisted designs (transparent and easy to implement, excellent performance. For example: mTPI, BOIN, keyboard design).
Regarding the limitations of the 3+3 design, Professor Yuan summarized the following five points:
1. Low efficiency in accurately identifying the MTD
2. Cannot define a specific target DLT
3. Unable to make dose escalation or de-escalation decisions for cohorts other than sizes of 3 or 6
4. Unable to remain logically and scientifically consistent with cohort expansions
5. May easily result in patients receiving subtherapeutic doses
Regarding optimal decision-making, Professor Yuan candidly stated that a perfect design does not exist, and decisions must be made based on a large accumulation of data. The BOIN design, which minimizes the possibility of erroneous decisions and approaches the perfect design while remaining exceptionally simple, is undoubtedly the best solution.
"Simplicity is the ultimate sophistication", Professor Yuan used Leonardo da Vinci's famous quote and the typical rules from Steve Jobs's design philosophy to explain the principles upheld by the BOIN design—simplicity, transparency, and good statistical and operational characteristics.
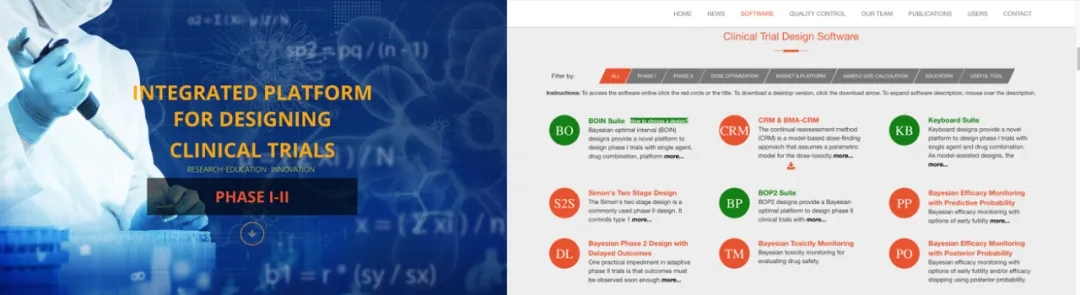
www.trialdesign.org
◎ Topic: Key Considerations in External Control Trial Design and Case Applications

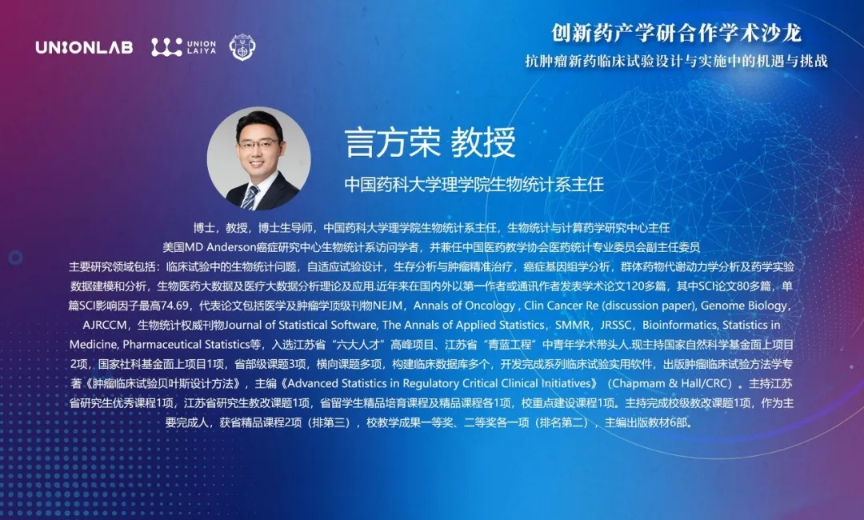
Professor Fangrong Yan
School of Sciences, China Pharmaceutical University
Head of the Department of Biostatistics
Professor Fangrong Yan is a Ph.D., Professor, Doctoral Supervisor, Head of the Department of Biostatistics at the School of Sciences, China Pharmaceutical University, Director of the Biostatistics and Computational Pharmacy Research Center, Visiting Scholar at the Department of Biostatistics, MD Anderson Cancer Center, USA, and concurrently serves as Deputy Chairman of the Medical Statistics Professional Committee of the China Medical Teaching Association. His main research areas include biostatistical issues in clinical studies, adaptive trial design, survival analysis and precision oncology, cancer genomics analysis, population pharmacokinetics analysis, modeling and analysis of pharmaceutical experimental data, biomedical big data, and theories and applications of medical big data analysis. In recent years, he has published over 120 academic papers as the first author or corresponding author domestically and internationally, including more than 80 SCI-indexed papers, with the highest single SCI impact factor of 74.69. Representative papers include publications in top medical and oncology journals such as NEJM, Annals of Oncology, Clin Cancer Re (discussion paper), Genome Biology, AJRCCM, and authoritative biostatistics journals such as Journal of Statistical Software, The Annals of Applied Statistics, SMMR, JRSSC, Bioinformatics, Statistics in Medicine, and Pharmaceutical Statistics. He was selected for Jiangsu Province's "Six Talent Peaks" project and the "Qinglan Project" as a young and middle-aged academic leader. Currently, he is leading two general projects of the National Natural Science Foundation of China, one general project of the National Social Science Fund, three provincial and ministerial-level projects, and multiple collaborative projects. He has built multiple clinical databases, developed a series of practical software for clinical studies, published the monograph "Bayesian Design Methods for Oncology Clinical Studies," and served as editor-in-chief of "Advanced Statistics in Regulatory Critical Clinical Initiatives" (Chapman & Hall/CRC). He has led one excellent graduate course in Jiangsu Province, one graduate education reform project in Jiangsu Province, one provincial boutique cultivation course and boutique course for international students, and one key construction course at the university level. He has led and completed one university-level educational reform project, and as a main contributor, received two provincial-level boutique courses (ranked third), and won one first prize and one second prize in university teaching achievements (ranked second). He has edited and published six textbooks.
As clinical studies continue to deepen, randomized controlled trials (RCTs), although considered the gold standard for evaluating interventions, still have certain limitations. For example, difficulties in participant enrollment, challenges in implementing control group designs for rare or major diseases, long study durations, and high costs.
Therefore, another method to assist in overcoming the limitations of RCTs—the Real-World Evidence (RWE) study—has emerged. How to use RWE to evaluate the efficacy and safety of drugs in the fields of drug development and regulation has become a hot topic of common concern among global regulatory agencies, industry, and academia.
When discussing external control trial design, Professor Yan pointed out that the most important consideration is the control of bias, while population, treatment, follow-up time, and endpoints are crucial factors to consider at the design level.
Professor Yan also conducted an in-depth analysis of the statistical analysis for external controls. He considered that there is no single specific method suitable for all external control trials, and the FDA recommends proposing methods based on the specific circumstances of the trial. It is necessary to identify and control confounding factors and bias, including differences in baseline factors and confounding variables between trial groups. Planning is required, using quantitative or qualitative bias analyses to assess the impact of confounding factors and bias, and considering the expected effect size of the primary endpoint. When the expected effect size is not large, bias may affect the results; if inappropriate, additional analyses should be conducted to assess the comparability of important covariates between the external control group and the treatment group.
Finally, through case analysis, Professor Yan considered that in the process of drug development, utilizing and analyzing RWD to generate clinical evidence related to the use of medical product use and potential benefits or risks can reduce R&D costs and the burden on patients. As long as regulatory requirements are met, it is expected that in the future, the proportion of clinical studies using RWE will increase, with a wider scope of application. Factors that the FDA focuses on when evaluating RWE include: whether the RWD is applicable (whether the clinical research methods are acceptable, and whether the data is reliable and relevant), whether the study design used to generate RWE can provide sufficient scientific evidence to answer regulatory questions, and whether the study implementation complies with the FDA's regulatory requirements.


Q1: What are the considerations for the design of cohort sample sizes?
Answer: In the BOIN design, patient allocation is adaptively adjusted based on data. However, we often terminate early; generally, 12 is an appropriate sample size. If you want to expedite the study, it can be set to 9.
Q2: In indication expansion and post-marketing studies initiated by investigators, when comparing real-world data with historical data yields better results, what are the key statistical considerations of the CDE and FDA?
Answer: There are no explicit considerations.
Q3: What precautions should be taken before conducting external control trials?
Answer: First, the sponsor needs to solidify the preliminary research work to clarify whether the conditions for conducting the trial are met. With a solid foundation in place, then proceed to discuss with the CDE to determine the feasibility of these conditions.
Q4: For projects using external control methods other than the conventional Phase I, II, and III trials, is additional communication with the CDE necessary?
Answer: Regular communication is sufficient. However, it is recommended to list and compare important factors before conducting the trial to ensure its smooth progress.
Q5: It is acceptable to reset after bridging therapy and before cell therapy. If an externally designed study has been approved by the CDE, is there an innovative statistical method to avoid interference from external drugs on the control and experimental groups?
Answer: First, evaluate how much the new external intervention helps the drug's efficacy. If it only involves safety issues and does not affect efficacy, then there's no problem. If it affects the efficacy evaluation, the estimation of efficacy needs to be corrected. Cell therapy involves two steps: the first step is the efficiency of peripheral blood (i.e., whether the cells have expanded); the second step is to evaluate the objective efficacy. There is significant individual variability in cell therapy, and the CDE also hopes to obtain some data in humans, so it is recommended to continue collecting data subsequently.
Q6: Have the BOIN-Comb or Waterfall designs been used in previous studies? I did not find any relevant case studies on Clinical Studies.
Answer: Yes. In a certain domestic CAR-T drug, before CAR-T therapy, a premedication (interleukin) is used for depletion, i.e., Comb. The above design is used in many studies in the United States.
Q7: Have the BOIN-Comb or Waterfall designs been used in previous studies? I did not find any relevant case studies on Clinical Studies.
Answer: Yes. There is a CAR-T drug in China, which uses a preconditioning drug (interleukin) to perform lymphodepletion (Comb) before CAR-T therapy; many studies in the United States are using the above design.
Q8: In the BOIN12 design, besides toxicity, efficacy is also considered. How do we estimate the sample size for efficacy?
Answer: Generally, there are two methods. The first suggests setting the initial sample size as 6 times the number of dose levels, which can be understood as the maximum sample size in a 3+3 design; the second is to use software to simulate the maximum sample size.
Q9: For preliminary efficacy analysis in Phase Ib & II, what is the recommended sample size for backfill consideration? We hope to select two dose levels and the optimal indication among two indications.
Answer: It depends on whether you are comparing these two doses or exploring efficacy along the lines of a Phase II study. If addressing dose optimization, the FDA recommends conducting a randomized exploration of the optimal dose(s) within one or more doses; recent theoretical analyses suggest enrolling 20–40 patients. This is similar to the sample size in Simon's two-stage design. Of course, it also depends on how large the differences are between the dose groups to be tested, and how much Type I error rate and power you wish to control.

PI Perspective: Challenges of Statistical Application in Clinical Studies
(including BOIN Design)
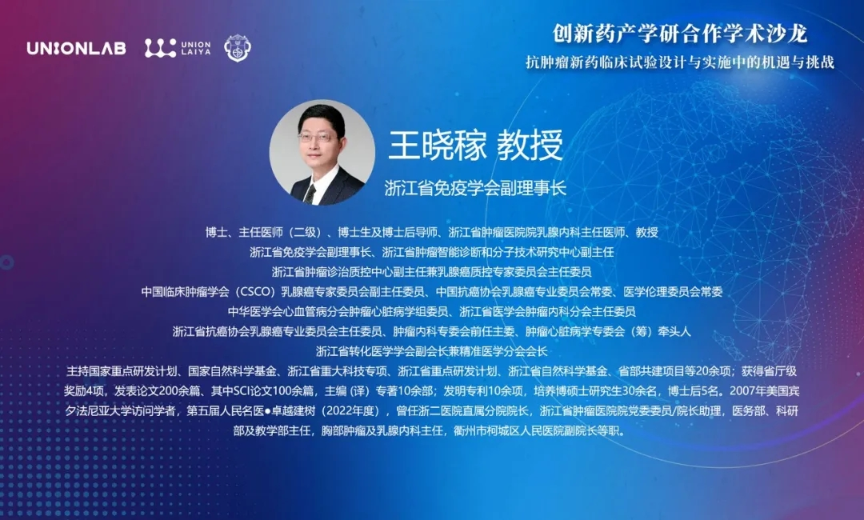
Professor Xiaojia Wang, Vice President of Zhejiang Society of Immunology
Professor Xiaohua Liang, Director of the Department of Oncology, Huashan Hospital Fudan University
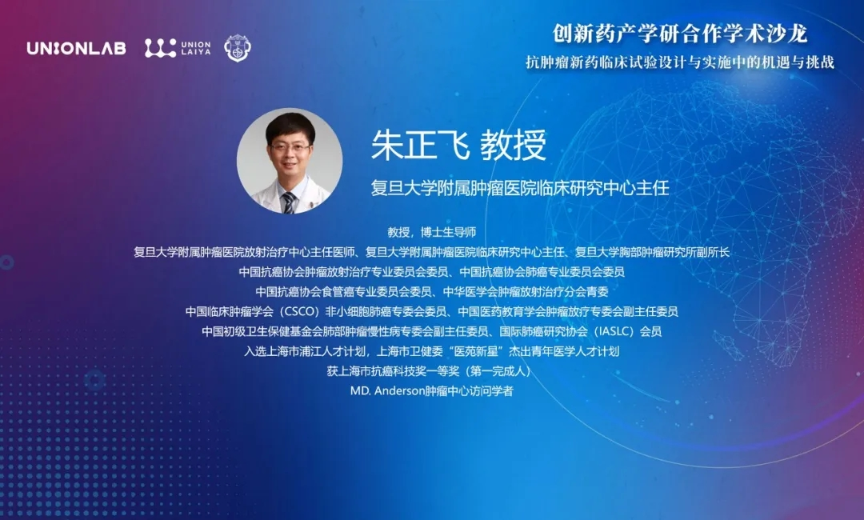
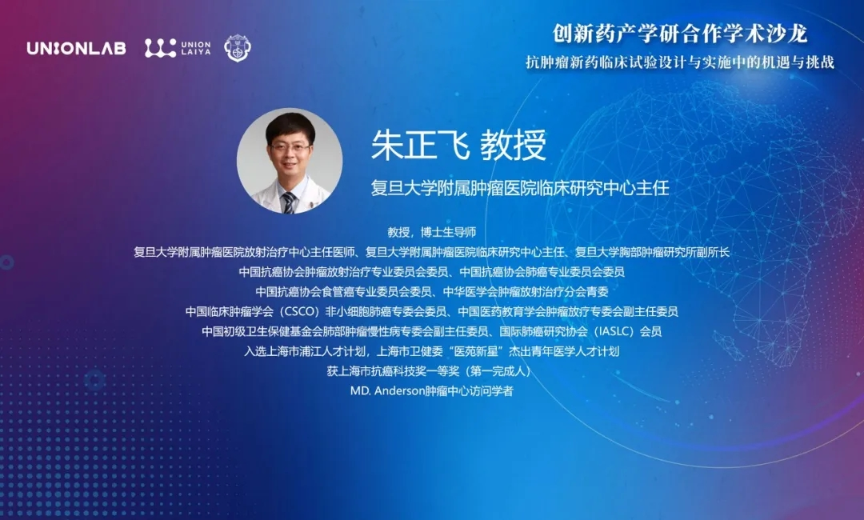
Professor Zhengfei Zhu, Director of the Clinical Research Center, Fudan University Shanghai Cancer Center


1. May I ask each PI, besides the traditional 3+3 design, are there any other designs you can share? What difficulties have you encountered?
Professor Wang: Success depends on statistics, and failure also depends on statistics. For a PI, the responsibility is tremendous; once a problem occurs, it can lead to project termination. We generally conduct single-arm or Phase I and II bridging studies. During dose escalation in Phase I, we consult statistical experts to solve clinical issues.
Professor Zhu: In Phase I studies, many companies choose the 3+3 design. However, some foreign companies opt for the BOIN design or start Phase Ib expansion simultaneously during Phase Ia, such as in the same dose group, increasing sample size, and combination therapies. Future research development may head in two directions: the first is based on master protocol designs. In the future, sponsor-initiated studies with master protocol designs may face difficulties, whereas IITs and CRO-initiated studies might pass more easily. Secondly, adaptive systems and AI will certainly accelerate the development of clinical research. Can we use existing clinical research data of similar drugs to simulate survival curves through AI methods and then analyze them using the BOIN design?
Professor Liang: First, we need to clarify what issues can be resolved before considering which statistical method to choose. The BOIN design is particularly suitable for immunotherapy (especially cellular immunotherapy) and multi-target drugs.
Professor Yuan: Statistics and medicine are, to some extent, a collaboration. A successful design must be the result of close cooperation between statisticians and clinicians, and it is also a process of mutual assistance.
Professor Yan: Clinical research is a combination of science and art. Biostatisticians assist clinicians in answering questions with data, which requires prior planning rather than post-hoc remedies.
2. Regarding changes in the efficacy and safety of BOIN12, when patients withdraw from the group but it is necessary to obtain drug efficacy data, how should the design be adjusted?
Professor Wang: For 21-28 days after a patient experiences DLT, they should be managed according to clinical treatment protocols, and no interventions should be made during this period. Whether to re-administer the drug should be considered when designing the trial.
Professor Zhu: The fundamental principle of clinical studies should be patient-centered, considering both safety and efficacy. First, we need to judge based on the actual situation whether it is appropriate for the subjects to continue into Phase III. Second, we cannot, in order to save costs, regard the efficacy data obtained from beneficial medication after DLT occurrence as valid data. We should proceed according to the initial study design.
3. From the perspective of the three experts, what factors need to be considered when communicating with various parties to effectively conduct clinical studies?
Professor Wang: It is necessary to repeatedly discuss and communicate with statisticians throughout the process, and the implementation plan must pass ethical review. After data emerges during the process, we still need to repeatedly discuss whether adjustments are needed.
Professor Zhu: Currently, the domestic pharmaceutical investment field is intensely competitive. For sponsors in China, the most important aspect is to grasp the forward-looking nature of drugs, which requires an in-depth understanding of the market for similar drugs.
Professor Liang: At present, oncology clinical research is still dominated by traditional methods. We should learn and embrace new technological approaches and statistical methods.

Discussion Session: Bayesian Methods in Oncology Clinical Studies
Opportunities and Challenges in Practical Application within China
Professor Ying Yuan, Bettyann Asche Murray Distinguished Professor, Associate Head of the Department of Biostatistics, MD Anderson Cancer Center, USA
Professor Fangrong Yan, Head of the Department of Biostatistics, School of Science, China Pharmaceutical University
Professor Xiaojia Wang, Vice President of Zhejiang Society of Immunology
Professor Xiaohua Liang, Director of the Department of Oncology, Huashan Hospital Fudan University
Professor Zhengfei Zhu, Director of the Clinical Research Center, Fudan University Shanghai Cancer Center
Professor Qun Li, Director of Education at the Oncology Center, Shanghai East Hospital Tongji University
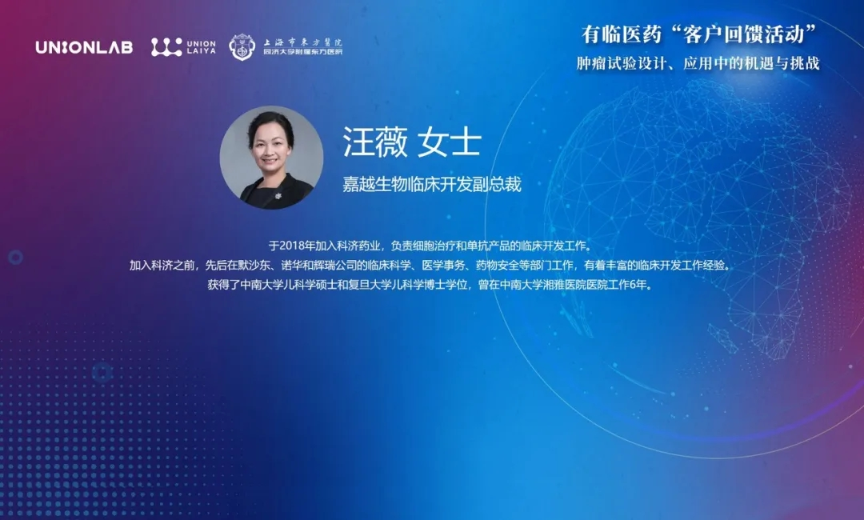
Dr. Wei Wang, Vice President of Clinical Development, Jiayue Biotech
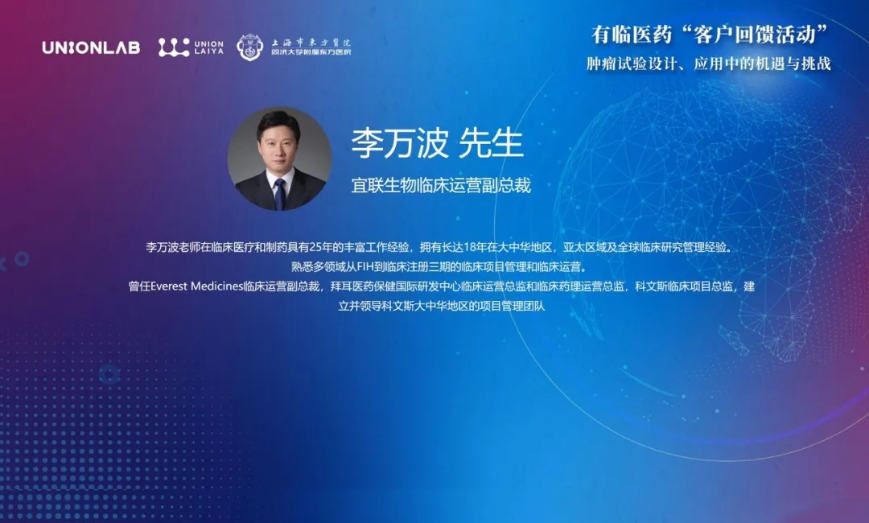
Mr. Wanbo Li, Vice President of Clinical Operations, Medilink Thera
Dr. Haixiong Han, Chief Medical Officer and Registration Director of
Mr. Lei Zhang, Senior Director of Biostatistics, Union Laiya





1. Despite the numerous documents issued by the FDA and CDE regarding real-world studies, based on the current domestic situation, we are consistently perplexed about the completeness and reliability of data sources. Electronic medical records cannot provide much valuable reference data. How can we resolve such issues?
Professor Fangrong Yan: Actually, when regulatory authorities in various countries issue a series of guidelines, they also hope to provide us with more tools to choose from. However, the data source is indeed a common problem in real-world research and external control designs. It is recommended to implement such studies only when there is at least an 80% chance of successful execution.
Professor Ying Yuan: Firstly, as a forward-looking consideration, regulatory agencies are also collecting and storing today's data for the future, striving to ensure its completeness and reliability as much as possible. Secondly, we can use some innovative designs to alleviate such problems, such as hybrid studies. By not fully trusting the reliability of external data, we compare its bias with internal data and then make adaptive adjustments.
2. Regarding the use of the BOIN design in early-stage projects, could you please share your experiences and feedback?
Director Qun Li: Since Professor Jin Li came to the East Hospital in 2017, the center began carrying out clinical research projects. Currently, there are over 300 studies from Phase I to Phase III, with IIT studies accounting for about 10%. Generally, we follow the sponsor's design methods, and the BOIN design accounts for less than 10%. However, compared to the 3+3 design, the error rate is very low. In the past, clinical and basic research operated independently, but now, like in the United States, statisticians and clinicians continually communicate and discuss together. This reflects that China's clinical studies are gradually learning from excellent Western models.
Dr. Wei Wang: In the past, when dose exploration was conducted in cell therapy, considering that each patient was hard to come by and the high costs involved and that the abundant literature was available in the field of cell therapy for reference, we chose the 3+3 design at that time. Now, among the seven targeted small molecule drugs developed by Jiayue Biotech, the latest one adopts the BOIN design. I would also like to ask Professor Yuan, if we use the BOIN design to first obtain the MTD, can we determine the dosing standards through clinical decision-making? Additionally, are there any statistically helpful methods for dose titration?
Professor Ying Yuan: Regarding dosing standards, there is actually a 2-Stage design. In Stage 1, a safe dose range is found through dose escalation; in Stage 2, optimal dose groups are selected for dose expansion, and finally, a more appropriate dose is chosen. Dose titration requires a more complex design approach.
Mr. Wanbo Li: In the Phase I clinical studies I have participated in, besides the traditional 3+3 design, some projects have used the BOIN design. For startup companies, especially when conducting global clinical projects, in addition to comprehensive protocol design, project operators need to have strong project management and coordination capabilities. From some current trial data in the industry, the BOIN design can indeed reduce the number of patients compared to the traditional 3+3 design, shortening the Phase I development time.
Dr. Han Haixiong: In recent years, has also encountered many projects similar to Real World Studies or innovative design projects. Although the foundational data in China's pharmaceutical field still has a long way to go, I personally believe that Real World Studies can still provide references for companies when conducting key clinical designs and estimating sample sizes. Additionally, regarding innovative designs, whether it's the 3+3 design or the BOIN design, it's best to choose based on one's own needs (drug characteristics, classification, indication selection, budget, and plan).
3. If a DLT is found in a dose group, even if there are doubts about it but it is still acknowledged, how should subjects be enrolled? According to BOIN rules, if 1 out of 4 or 5 people experiences a DLT, we can continue, so we proceed to enroll 1 or 2 more people. Experts, is such a design reasonable?
Professor Ying Yuan: It is reasonable. Because clinicians do not only look at a single DLT but consider the entire safe dosage range, we recommend everyone use the BOIN design.
4. When conducting global Phase I and II dose-escalation trials, by relatively independently separating back-fill and dose-escalation subjects, and when finally deciding on escalation or de-escalation, aggregating all data and making the final decision primarily based on dose-escalation data supplemented by back-fill data. May I ask the experts whether this is feasible?
Professor Ying Yuan: At least it's not very ideal. From an ethical perspective, if the dose is safe during escalation but DLT appears during backfill, it would be unreasonable to continue escalating the dose; all data should be aggregated before making further considerations. Regarding how to use the BOIN design in the backfill to handle this both perfectly and simply, we are also accelerating our research and look forward to sharing it with everyone as soon as possible.
5. If there is no DLT during BOIN dose escalation, but one out of three patients in the backfill experiences DLT, this patient will not affect the dose escalation decision, right?
Professor Ying Yuan: Correct, this is an individual case, no problem.
6. If the three additional patients do not experience DLT during the observation period, but DLT occurs during long-term medication, how should experts handle this?
Professor Zhengfei Zhu: This is why we need to conduct Phase IV studies after completing Phase III research.
Professor Ying Yuan: Actually, the handling of backfill and dose escalation is the same. If DLT occurs (even during long-term medication), it is recommended that sponsors and investigators consider conservatively and not rashly escalate to the next dose level.
Director Qun Li: It still depends on what kind of toxicity it is. Safety should be the priority, patient-centered, and not just to rush for aggressive market approval.
The four-plus-hour exchange passed in a flash, but the reflections it left for medical professionals have never ceased. As the development speed of domestic pharmaceutical companies continues to accelerate, China now possesses world-class clinical research teams. Intelligent technologies have further improved efficiency, and the gap with international counterparts has gradually narrowed. It is an inevitable trend for original innovative drugs to venture abroad, but this also poses new challenges to the multi-party win-win model. For innovation to go overseas, it needs to return to the patients themselves and requires deep cooperation among all participants. also hopes to continue persisting in doing what is difficult but right, to collaborate with industry peers to grow stronger together and overcome challenges.